Uncovering the Unseen Threat: Seasonal Patterns and Enduring Resistance
The global health crisis of antimicrobial resistance (AMR) poses a grave danger, jeopardizing progress in medicine, food production, and life expectancy worldwide. Despite its paramount importance, limited data on population-level prevalence, including seasonal and temporal variations, hampers accurate risk assessment for AMR transmission. This study delves into the temporal dynamics and persistence of resistance genes within an urban community, providing valuable evidence to guide AMR control policies and promote responsible antibiotic/antimicrobial use.
Wastewater-Based Epidemiology: A Window into Community-Acquired Resistance
The study employed a temporal strategy, utilizing sewage (wastewater-based epidemiology—WBE) to evaluate the prevalence, abundance, and dynamics of resistance over a 5-month period. Quantitative real-time PCR (q-PCR) was used to analyze 123 antibiotic resistance genes (ARGs) and 13 mobile genetic elements (MGEs) in the wastewater of a selected urban community.
Key Findings:
Persistent Resistance Dominates the Landscape
– Approximately 50% of the tested ARG subtypes were consistently detected in all months, with a frequency ranging from 52 to 61%.
– The winter months (December and January) exhibited the maximum absolute abundance of resistance genes.
– Detected clinically significant genes (ndm-1 and cfiA) and other variants (blaoxy, aph, aacC, tet-35, tet M, tet-32) can confer resistance to 3rd and 4th generation β-lactam, aminoglycoside, tetracycline, and multidrug classes, contributing significantly to core/persistent resistance.
Seasonal Fluctuations Shape Resistance Dynamics
– ARGs encoding resistance to aminoglycosides, sulfonamide & trimethoprims, and β-lactams consistently demonstrated high resistance levels throughout the sampling period.
– The absolute and relative abundance of ARGs and MGEs peaked during the winter months, with a progressive decline towards the summer.
– This seasonal pattern aligns with the increased antibiotic usage and bacterial activity observed in colder seasons, underscoring the critical role of environmental factors in shaping resistance dynamics.
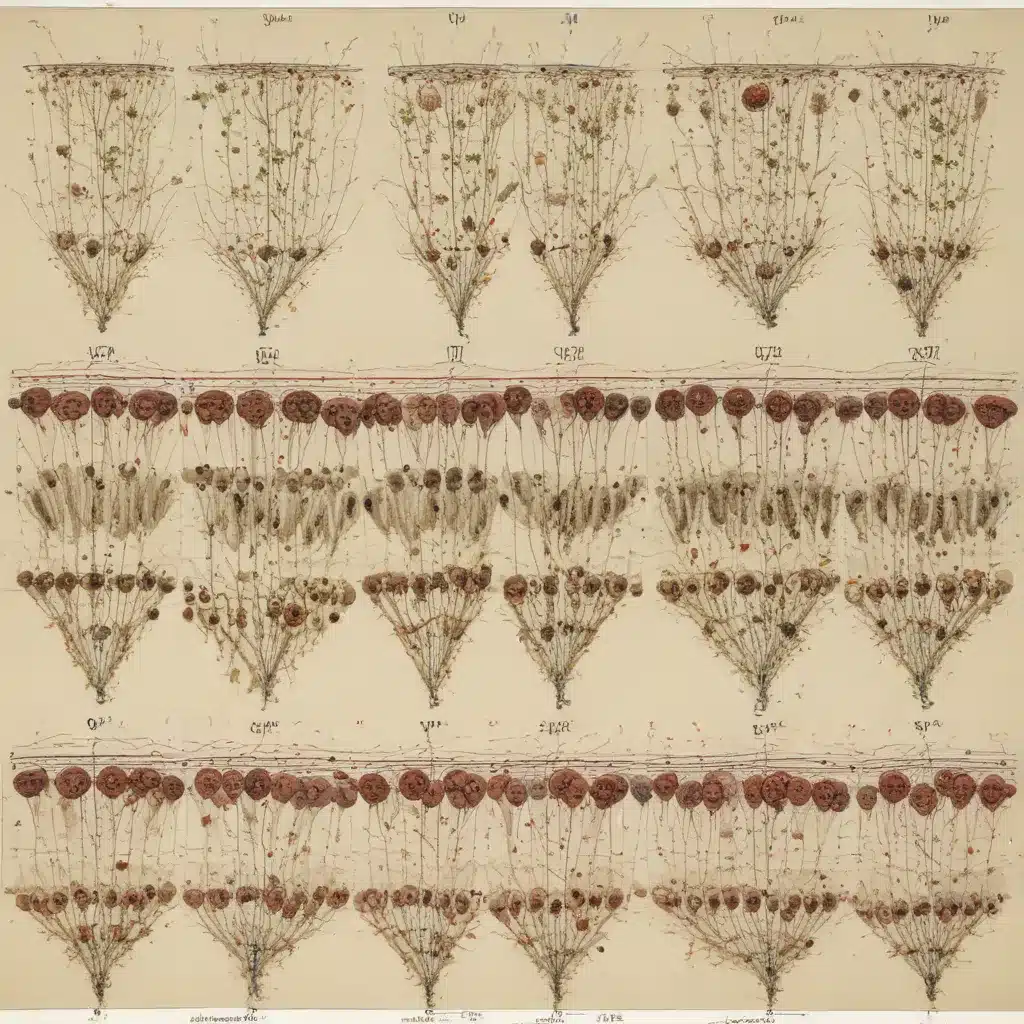
Co-Abundance Reveals Resistance Gene Transmission Pathways
– Network analysis of co-abundant ARGs and MGEs identified significant and robust correlations, suggesting a high likelihood of resistance transmission within the study site through horizontal gene transfer.
– Clusters of ARGs conferring resistance to the same antibiotic classes were observed within distinct modules, indicating shared distribution patterns and functional associations.
Implications for AMR Mitigation and Responsible Antibiotic Use
This study provides a comprehensive understanding of temporal resistance dynamics in an urban environment, bridging a crucial gap in the global knowledge on AMR. The insights gained can inform community-oriented AMR strategies, clinical decision-making, and early disease outbreak detection.
The detection of clinically significant resistance genes and the predominance of persistent resistance underscore the urgent need for enhanced urban resistance surveillance and targeted interventions. Policymakers and public health authorities can leverage these findings to develop evidence-based AMR control policies and promote the responsible use of antibiotics and antimicrobials, ultimately preserving their effectiveness for future generations.
By shedding light on the seasonal patterns and enduring nature of resistance genes, this research equips water and sanitation professionals, community advocates, and public health practitioners with the knowledge to tackle the complex challenge of AMR in urban settings. Empowered with this understanding, stakeholders can make informed decisions, implement tailored strategies, and foster collaborative efforts to safeguard our communities and the environment from the growing threat of antimicrobial resistance.
Navigating the Seasonal Ebb and Flow of Resistance
Uncovering the Resistance Landscape
The study area, an urban community in Hyderabad, India, was selected based on insights from a previous investigation conducted by the research team. This locale, with a population of around 1.8 lakh and a daily wastewater flow of 27 ± 2 MLD, was found to have a high magnitude of resistance in the earlier study. The current research aimed to elucidate the temporal dynamics of antibiotic resistance genes (ARGs) and mobile genetic elements (MGEs) within this community.
Wastewater samples were collected monthly over a 5-month period, from December 2021 to April 2022, covering the winter and summer seasons. Using quantitative real-time PCR (q-PCR), the researchers analyzed 123 ARGs and 13 MGEs, representing resistance to a wide range of antibiotics, including β-lactams, tetracyclines, aminoglycosides, and more.
Persistent Resistance: The Core of the Problem
Approximately 50% of the tested ARG subtypes were consistently detected in all five months, with a frequency ranging from 52 to 61%. This persistent resistance, characterized by the widespread presence of ARGs across various classes, is of particular concern.
The researchers identified clinically significant genes, such as ndm-1 and cfiA, which confer resistance to carbapenems – considered the last-resort antibiotics. Additionally, they found variants like blaoxy, aph, aacC, tet-35, tet M, and tet-32, which can impart resistance to 3rd and 4th generation β-lactams, aminoglycosides, and tetracyclines. These genes contribute significantly to the core, or persistent, resistance observed in the community.
Seasonal Dynamics: Resistance Peaks in Winter
The temporal analysis revealed that the absolute abundance of ARGs and MGEs was highest during the winter months of December and January, with a progressive decline towards the summer.
Key Observations:
- Aminoglycosides, sulfonamide & trimethoprims, and β-lactams consistently demonstrated the highest resistance levels throughout the sampling period.
- Moderate resistance was observed for multidrugs, MLSBs, and tetracyclines, while chloramphenicols and quinolones exhibited lower resistance.
- The number of detected ARG subtypes was highest in March and lowest in December, reflecting the seasonal variations.
This seasonal pattern aligns with the increased antibiotic usage and bacterial activity typically observed in colder seasons. The stress-induced SOS response and enhanced genetic recombination during winter months may also contribute to the elevated detection of resistance genes and mobile genetic elements.
Resistance Gene Transmission: A Network Perspective
Network analysis of the co-abundance patterns among ARGs and MGEs revealed significant and robust correlations, suggesting a high likelihood of resistance transmission within the study site through horizontal gene transfer.
The researchers observed that ARGs conferring resistance to the same antibiotic classes tended to cluster together within distinct network modules. This indicates shared distribution patterns and functional associations among the resistance genes, highlighting the potential pathways for resistance gene dissemination.
The identification of highly interconnected “hub” genes, such as lnuB, penA, mphA-02, and cmlA1-01, underscores their pivotal role in the persistence and spread of resistance within the community.
Implications for AMR Mitigation
The findings of this study provide valuable insights to guide antimicrobial resistance (AMR) control policies and promote the responsible use of antibiotics and antimicrobials. The detection of clinically significant resistance genes and the predominance of persistent resistance emphasize the urgent need for enhanced urban resistance surveillance and targeted interventions.
Policymakers and public health authorities can leverage these insights to develop evidence-based strategies that address the seasonal fluctuations and enduring nature of resistance genes. This can include tailoring antibiotic prescription guidelines, implementing seasonal monitoring programs, and raising awareness among healthcare professionals and the community about the importance of responsible antibiotic use.
By understanding the temporal dynamics and persistence of resistance genes, water and sanitation professionals, community advocates, and public health practitioners can make informed decisions, implement effective mitigation strategies, and foster collaborative efforts to combat the growing threat of AMR in urban settings.
Conclusion: Empowering Communities to Confront the AMR Challenge
This study’s comprehensive investigation of temporal resistance dynamics in an urban community provides a crucial foundation for addressing the global challenge of antimicrobial resistance. The insights gained shed light on the seasonal patterns and persistent nature of resistance genes, equipping stakeholders with the knowledge to develop targeted interventions and promote responsible antibiotic use.
By understanding the trends in resistance gene prevalence and the role of environmental factors, policymakers and public health authorities can design more effective AMR control policies and surveillance programs. Water and sanitation professionals, alongside community advocates, can leverage this knowledge to implement tailored strategies that safeguard urban environments and empower communities to take an active role in combating the AMR crisis.
Through collaborative efforts and evidence-based decision-making, we can navigate the seasonal ebb and flow of resistance, ultimately preserving the effectiveness of antibiotics and safeguarding the health and well-being of communities worldwide.

