Unveiling the Molecular Landscape of Osteoarthritis Progression
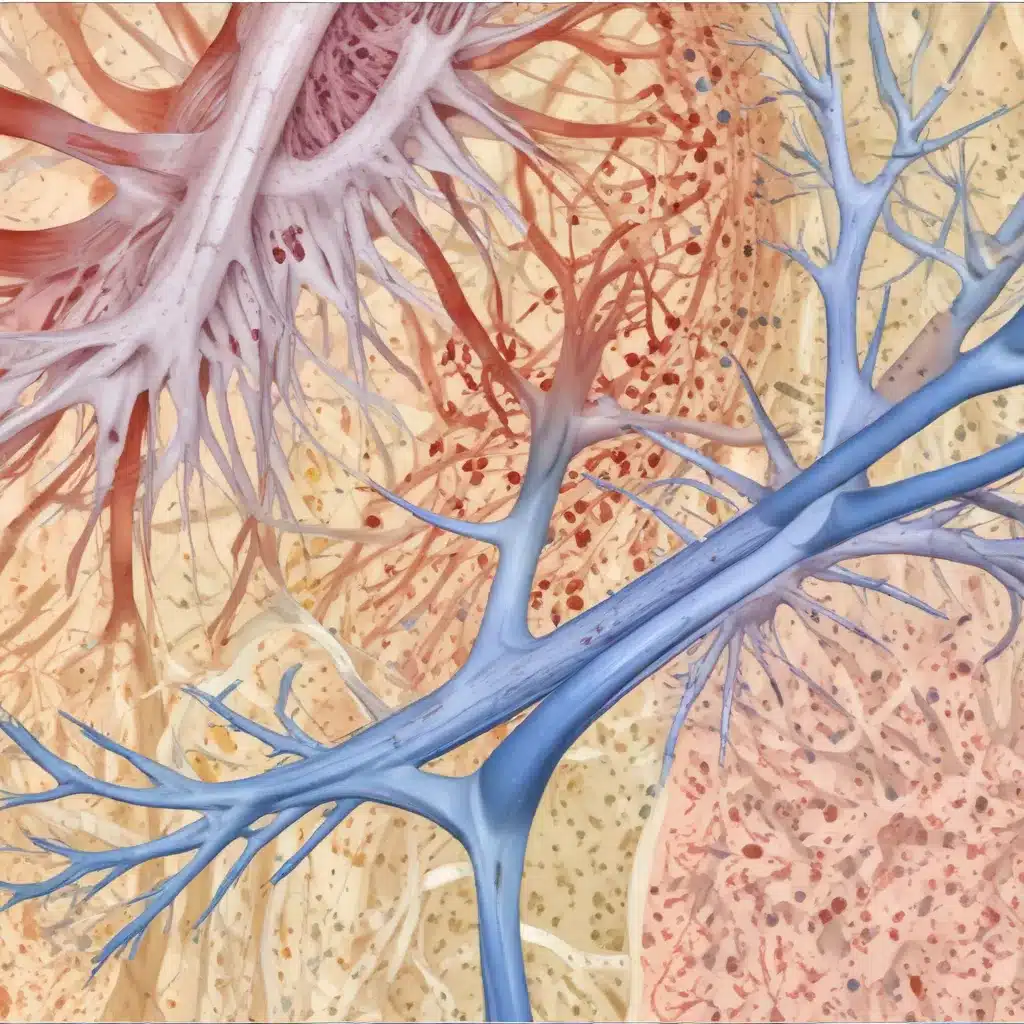
Osteoarthritis (OA) is the most prevalent degenerative joint disorder, characterized by progressive cartilage loss, subchondral bone changes, and synovial inflammation. Understanding the intricate molecular mechanisms underlying OA progression is crucial for developing effective diagnostic tools and therapeutic interventions. Recent advancements in transcriptomic profiling have shed light on the dynamic alterations in the synovial fluid, which serves as a reservoir for the joint’s molecular signatures.
In a comprehensive study published in the preprint server bioRxiv, researchers from the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, delved into the synovial fluid transcriptome across different stages of OA progression. By analyzing samples from patients with varying Kellgren-Lawrence (KL) grades, the team uncovered distinct gene expression patterns and associated pathways that evolve as the disease advances.
Key Findings and Insights:
-
AMTN and DKK2 Upregulation in Late-Stage OA: The study identified the consistent upregulation of two genes, AMTN and DKK2, with the progression of OA. AMTN, typically expressed in enamel-forming ameloblasts, was found to be significantly elevated in advanced OA (KL grade 4) compared to early-stage disease (KL grade 2). Similarly, DKK2, a Wnt signaling antagonist involved in osteoblast differentiation, also showed a substantial increase in late-stage OA. These findings suggest that pathological mineralization and disrupted bone remodeling play crucial roles in the severity of OA.
-
MSLN Downregulation Indicates Impaired Bone Remodeling: In contrast to the upregulated genes, the researchers identified MSLN (mesothelin) as the top downregulated gene in late-stage OA. Mesothelin is known to be involved in bone remodeling, and its decreased expression in advanced OA indicates a potential disruption in the balance between bone formation and resorption, further contributing to the disease progression.
-
Altered Inflammatory Pathways during OA Advancement: The study’s pathway analysis revealed significant changes in immune response, inflammation-related pathways, and cellular processes, such as autophagy and programmed cell death, across different OA stages. Notably, the upregulation of defense response, innate immune response, and interferon signaling pathways in end-stage OA suggest an enhanced inflammatory state, potentially driven by microbial components or viral infections infiltrating the joint.
-
Mitochondrial Dysfunction and Impaired Autophagy: The researchers also found that mitochondrial dysfunction and impaired autophagy were linked to increased inflammation in advanced OA. The upregulation of pathways related to mitochondrial components and ATP production, along with the downregulation of autophagy and protein processing pathways, indicate a breakdown in cellular homeostasis that exacerbates the inflammatory environment in late-stage OA.
These findings highlight the dynamic and complex nature of OA progression, where alterations in mineralization, bone remodeling, inflammation, and cellular processes collectively contribute to the deterioration of joint health. By unveiling these molecular signatures, the study provides valuable insights for the development of novel therapeutic strategies targeting the key pathways and genes involved in the different stages of OA.
Translating Insights into Potential Interventions
The identification of AMTN and DKK2 as consistently upregulated genes, alongside the downregulation of MSLN, suggests that targeting pathological mineralization and disrupted bone remodeling could offer promising avenues for OA management. Interventions aimed at modulating these pathways may help slow down or even prevent the progression of the disease, particularly in its early stages.
Furthermore, the study’s emphasis on the role of inflammation in OA advancement indicates that therapies focusing on immune regulation and cellular homeostasis could be beneficial. Strategies to mitigate the upregulated inflammatory pathways, such as the defense response, innate immune response, and interferon signaling, may help alleviate the detrimental effects of chronic inflammation on joint tissues.
Addressing mitochondrial dysfunction and restoring autophagy processes could also be valuable therapeutic approaches. By supporting cellular energy production and removing damaged organelles, these interventions may help maintain the integrity of joint structures and reduce the inflammatory burden in advanced OA.
Implications for Clinical Practice and Future Research
The insights gained from this comprehensive synovial fluid transcriptome analysis have several important implications for clinical practice and future research:
-
Biomarker Development: The identified genes and pathways, such as AMTN, DKK2, and mitochondrial dysfunction, can be further explored as potential biomarkers for OA diagnosis, prognosis, and disease monitoring. Tracking the expression or activity of these molecular signatures in synovial fluid or other accessible samples may aid in the early detection of OA and guide personalized treatment approaches.
-
Targeted Therapeutic Strategies: The study’s findings provide a roadmap for developing novel disease-modifying OA drugs (DMOADs) that target the key pathways and molecules driving OA progression. Therapeutic interventions, such as modulating mineralization, bone remodeling, and inflammatory signaling, may offer new hope for slowing or even halting the advancement of this debilitating condition.
-
Combination Therapies: Given the complex and multifaceted nature of OA, a combination of interventions targeting different aspects of the disease, such as mineralization, inflammation, and cellular processes, may prove more effective than single-target approaches. Exploring synergistic therapeutic strategies could lead to more comprehensive and personalized management of OA.
-
Integrated Systems Biology Approach: The success of this study in uncovering novel molecular drivers of OA progression highlights the value of a systems biology approach that integrates multi-omics data, such as transcriptomics, proteomics, and metabolomics, to obtain a comprehensive understanding of the disease mechanisms. Applying this integrated approach to larger patient cohorts and across diverse joint tissues can further refine the understanding of OA pathogenesis and identify additional therapeutic targets.
By leveraging the insights from this synovial fluid transcriptome analysis, the scientific community and healthcare providers can work together to improve the management of osteoarthritis. Through the development of better diagnostic tools, targeted therapies, and personalized treatment strategies, the goal of enhancing the quality of life for individuals affected by this debilitating condition can be realized.
The Joint Action for Water blog is proud to share these cutting-edge findings and their implications for the water and sanitation sector. As we continue to advocate for improved community health and environmental sustainability, understanding the complex interplay between joint health, inflammation, and cellular processes can inform our approaches to holistic wellbeing. By bridging the knowledge gained in osteoarthritis research with our work in water and sanitation services, we can empower communities to address the multifaceted challenges they face.

