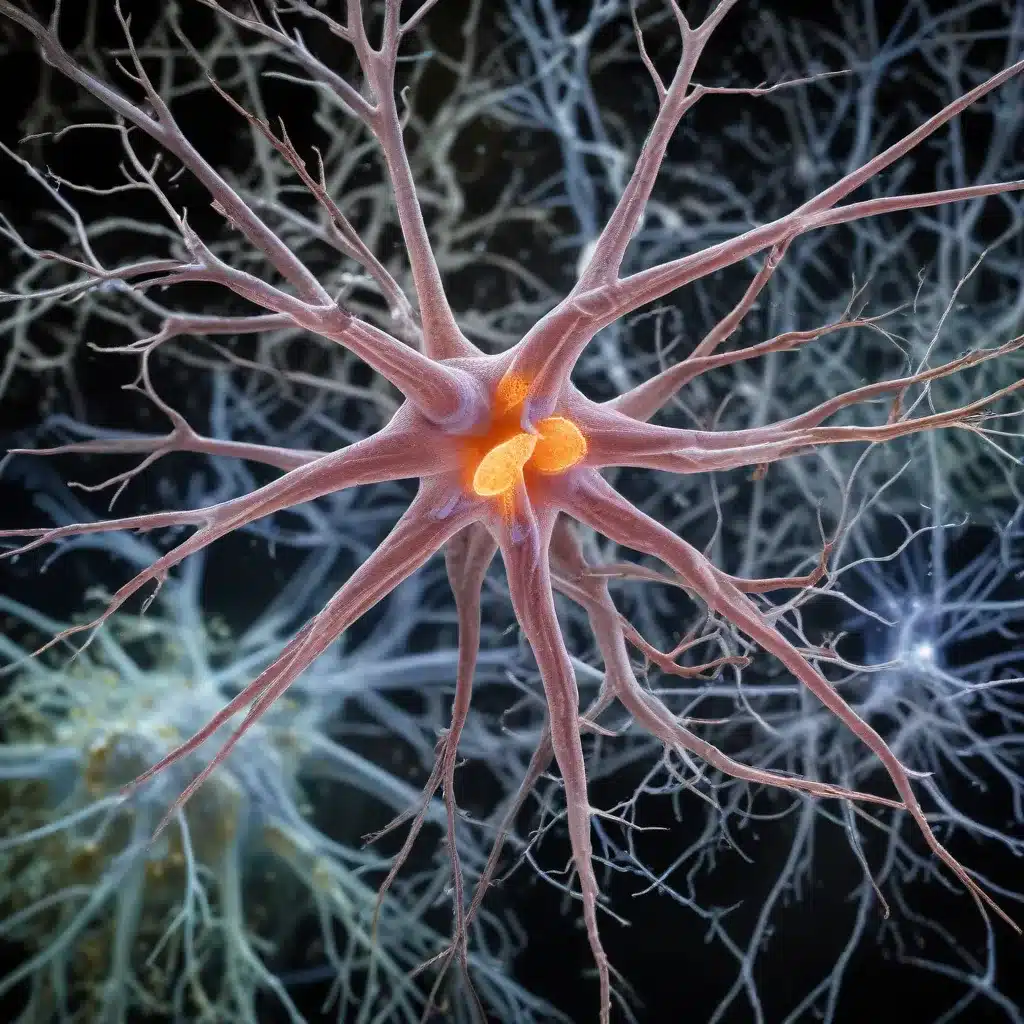
The Immune-Nervous System Interaction in Asthma
The immune and sensory nervous systems have evolved together, utilizing a shared language of receptors and transmitters to maintain homeostasis by responding to external and internal disruptions. While this interaction is beneficial in many cases, neurons can also exacerbate inflammation during allergic reactions, such as asthma.
Our research has modeled asthma aggravated by pollution, exposing mice to ambient PM2.5 particles and ovalbumin. This exposure significantly increased bronchoalveolar lavage fluid neutrophils and γδ T cells compared to exposure to ovalbumin alone. Interestingly, we were able to normalize airway inflammation and lung neutrophil levels by silencing nociceptor neurons at the peak of inflammation using intranasal QX-314 or by ablating TRPV1-expressing neurons.
Further investigation revealed heightened sensitivity in chemical-sensing TRPA1 channels in neurons from pollution-exacerbated asthmatic mice. Elevated levels of artemin, a member of the glial cell line-derived neurotrophic factor (GDNF) family, were also detected in the bronchoalveolar lavage fluid from pollution-exposed mice. Importantly, artemin levels returned to normal in mice with ablated nociceptor neurons.
Alveolar Macrophages: Key Orchestrators of Neurogenic Inflammation
Our in-depth analysis pinpointed alveolar macrophages as the source of artemin. These macrophages, which express the pollution-sensing aryl hydrocarbon receptor (AhR), responded to fine particulate matter (PM2.5) by releasing artemin. This molecule then enhanced TRPA1 responsiveness in vagal sensory neurons, leading to increased neutrophil influx and exacerbating airway inflammation.
These findings suggest a novel mechanism by which lung-innervating neurons respond to air pollution and highlight the potential of targeting this neuro-immune pathway as a therapeutic strategy for controlling neutrophilic airway inflammation in asthma, a clinically intractable condition.
Pollution-Exacerbated Asthma: An Emerging Challenge
Urban pollution and the increasing frequency and severity of wildfires contribute to higher concentrations of small particulate matter (less than 2.5 μm), shifting asthma from treatment-responsive eosinophilic and Th2-dominated types to treatment-resistant neutrophilic and mixed Th17/Th2 types. This form of asthma, characterized by significant neutrophilic infiltration, is often resistant to traditional treatments, highlighting a significant unmet need in respiratory healthcare.
Recent estimates suggest that neutrophilic asthma accounts for approximately 15–25% of all asthma cases, with around 50% of these cases being refractory to standard asthma treatments. Resolving neutrophilic asthma, therefore, constitutes an unmet clinical need of increasing importance.
Nociceptor Neurons: Key Players in Allergic Airway Inflammation
Our research, along with others, indicates that nociceptor neurons typically promote regulatory immunity in the context of bacterial, viral, or fungal infections, as well as in malignancies. However, the impact of neuro-immunity in regulating Th17 immunity in the lungs has been less explored.
In our model of pollution-exacerbated airway inflammation, we found that the ablation or silencing of nociceptor neurons prevented the induction of airway inflammation, highlighting a potential novel therapeutic pathway for treating refractory asthma. This finding echoes our previous preclinical data showing that nociceptor neuron silencing can stop eosinophilic airway inflammation.
Interestingly, we observed that ablating TRPV1 neurons, a subset of NaV1.8-expressing sensory neurons, decreased the influx of neutrophils exacerbated by pollution, suggesting a different underlying mechanism likely involving substance P rather than calcitonin gene-related peptide (CGRP).
Neuropeptides and Their Varied Immunomodulatory Effects
Emerging research highlights the diverse immunomodulatory effects of different neuropeptides. For instance, CGRP hinders the migration of dendritic cells in psoriasis, whereas substance P (SP) enhances their migration to lymph nodes in atopic dermatitis. Vasoactive intestinal peptide (VIP) and neuromedin U (NMU) increase the production of pro-asthmatic cytokines by lung ILC2 cells, whereas CGRP has similar or opposite effects.
In the lungs, CGRP reduces the infiltration of neutrophils and gamma-delta T (γδT) cells, offering protection against Staphylococcus aureus pneumonia. Conversely, CGRP can worsen psoriasis in the skin by inducing dendritic cells to produce IL-23, which activates IL-17-producing γδT cells, exacerbating inflammation.
Our findings indicate that nociceptor neuron ablation reduces γδ T-cell activation, an effect we attribute to SP/VIP-driven responses due to the lack of heightened CGRP release in our model. Future research will focus on how neurons directly regulate γδ T-cell and neutrophil function in these contexts.
The Aryl Hydrocarbon Receptor: A Critical Modulator of Inflammation
The aryl hydrocarbon receptor (AhR) is essential in modulating inflammation, as evidenced by its ability to decrease inflammation in the skin of psoriasis patients. Mice lacking AhR display worsened symptoms, underscoring its vital role in controlling inflammation.
Beyond its expression in alveolar macrophages, AhR is also present in various other innate immune cells, such as ILC2, eosinophils, and neurons. A recent preprint highlights AhR’s dual function as a critical molecular sensor and regulator, balancing neural protection and axon regeneration.
Although we have not formally tested this, it is plausible that AhR-expressing neurons, similar to alveolar macrophages, can directly sense fine particulate matter (PM2.5), potentially explaining the direct neuronal reprogramming we observed after pollutant exposure. Future research will explore this hypothesis using nociceptor neurons with conditional AhR knockout.
Artemin: A Key Mediator of Neurogenic Inflammation
Alveolar macrophages serve as an early warning system in the lungs, detecting pollutants like fine particulate matter and triggering defensive reflexes by releasing artemin. This action activates and sensitizes nociceptor neurons to TRPA1-sensing noxious stimuli.
Single-cell RNA sequencing revealed that a subtype of TRPA1, SST2R neurons, express the GDNF receptor GFRα3 and are sensitized by artemin. This finding complements previous research showing that keratinocyte-produced TSLP sensitizes skin-innervating nociceptor neurons, promoting itch and skin atopy.
In the lungs, TRPA1 germline knockout reduces allergic airway inflammation, while Genentech’s recent Phase 1 research demonstrated that TRPA1 agonists are elevated in asthmatic human airways and contribute to inflammation and hyperreactivity. Their development of GDC-0334, a selective TRPA1 antagonist, effectively reduces inflammation, cough, and allergic reactions in preclinical trials and decreases pain and itch in human studies, supporting TRPA1 sensitization and nociceptor neuron as a whole as a major upstream asthma driver.
Targeting the Neuro-Immune Axis: Novel Therapeutic Avenues
In the context of pollution-exacerbated asthma, our research links the sensitization of TRPA1+ nociceptor neurons and heightened allergic inflammation to artemin produced by macrophages. We propose new therapeutic targets to dampen neutrophilic airway inflammation by:
- Targeting the AhR-mediated pollution sensing by alveolar macrophages
- Inhibiting artemin’s effect on neurons by blocking GFRα3
- Blocking TRPA1 using novel antagonists such as GDC-0334
- Silencing nociceptor neurons with charged lidocaine derivatives
By interrupting this mechanistic pathway, we believe we can offer a novel approach to mitigating neutrophilic airway inflammation in pollution-driven asthma, a clinically challenging condition with significant unmet needs.
The Joint Action for Water blog is a valuable resource for the latest insights and practical advice on water and sanitation services, community engagement, and advocacy. Stay tuned for more informative articles on pressing environmental and public health issues.

