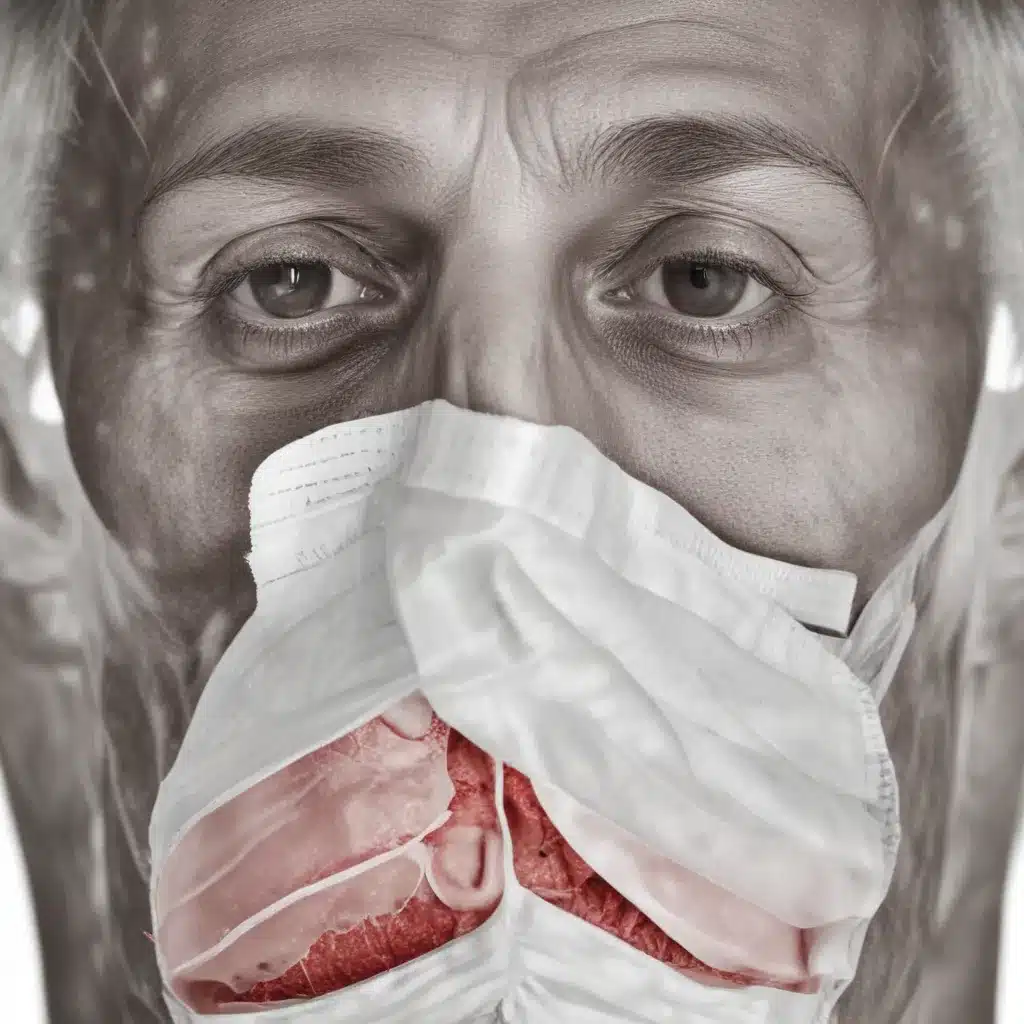
Tuberculosis: A Persistent Global Health Threat
Tuberculosis (TB) remains one of the world’s most pressing public health challenges, with a staggering impact on communities worldwide. Despite significant advancements in medical treatments and public health interventions, this ancient disease continues to plague millions, particularly in low- and middle-income countries. As a seasoned expert in water and sanitation services, community engagement, and advocacy, I am deeply committed to exploring the complex issues surrounding the management of TB and identifying strategies to address this persistent global health threat.
The Burden of Tuberculosis
Tuberculosis is a highly contagious, airborne disease caused by the bacterium Mycobacterium tuberculosis. According to the World Health Organization (WHO), in 2021, an estimated 10.6 million people fell ill with TB, and 1.6 million died from the disease. The burden of TB is disproportionately borne by low- and middle-income countries, with over 95% of TB deaths occurring in these regions. Factors such as poverty, malnutrition, and limited access to healthcare contribute to the high prevalence of TB in these vulnerable communities.
Challenges in Tuberculosis Management
The successful management of tuberculosis is hindered by a multitude of complex challenges, which require a holistic, collaborative approach to address. Some of the key obstacles include:
1. Drug Resistance
The emergence of drug-resistant strains of TB, such as multidrug-resistant (MDR-TB) and extensively drug-resistant (XDR-TB), has become a significant global concern. These resistant forms of the disease are more difficult to treat, often requiring longer, more intensive, and more expensive regimens. Inadequate access to quality-assured anti-TB drugs, poor adherence to treatment, and the misuse or overuse of antibiotics have all contributed to the rise of drug-resistant TB.
2. Barriers to Early Detection and Diagnosis
Timely and accurate diagnosis of TB is crucial for effective treatment and prevention of disease transmission. However, many individuals, particularly in resource-limited settings, face significant barriers in accessing diagnostic services. These barriers include limited availability of diagnostic tools, long distances to healthcare facilities, and the stigma associated with the disease, which can deter people from seeking care.
3. Comorbidities and Coinfections
The presence of comorbidities, such as HIV/AIDS, diabetes, and malnutrition, can significantly increase the risk of developing TB and complicate its management. These underlying conditions can compromise the immune system, making individuals more susceptible to TB infection and reducing the effectiveness of treatment. Coinfections, such as TB and HIV, also present unique challenges in terms of coordinating care and ensuring optimal treatment outcomes.
4. Socioeconomic Determinants
The management of tuberculosis is deeply intertwined with the socioeconomic conditions of affected communities. Poverty, lack of access to education, poor living conditions, and limited access to basic services, such as clean water and sanitation, can all contribute to the spread and perpetuation of TB. Addressing these underlying social determinants is essential for achieving sustainable progress in TB control.
5. Inadequate Funding and Resources
Effective TB control requires a robust and well-resourced public health infrastructure, including reliable supply chains, skilled healthcare workers, and comprehensive monitoring and evaluation systems. However, many high-burden countries face significant resource constraints, leading to gaps in service delivery and suboptimal TB management outcomes.
Strategies for Improved Tuberculosis Management
To address these multifaceted challenges, a comprehensive, collaborative, and multisectoral approach is necessary. Some key strategies for improving the management of tuberculosis include:
1. Strengthening Health Systems
Investing in the development of resilient and responsive health systems is crucial for effective TB control. This includes improving access to quality-assured diagnostic tools, ensuring the availability of essential anti-TB drugs, and providing comprehensive training and support for healthcare workers.
2. Fostering Community Engagement and Empowerment
Engaging with local communities is essential for enhancing TB awareness, promoting early case detection, and supporting treatment adherence. Empowering individuals and communities to take an active role in TB management can lead to more sustainable and equitable outcomes.
3. Addressing Social Determinants of Health
Tackling the underlying social, economic, and environmental factors that contribute to the TB burden is key to achieving long-term, sustainable progress. Interventions that improve access to education, clean water, and sanitation can have a profound impact on TB prevention and control.
4. Strengthening Collaborative Efforts
Effective TB management requires the collaboration of various stakeholders, including government agencies, international organizations, civil society, and the private sector. Fostering multisectoral partnerships and aligning strategies can help mobilize resources, share knowledge, and implement comprehensive interventions.
5. Investing in Research and Innovation
Continued investment in research and the development of new tools, technologies, and strategies is essential for advancing the global fight against tuberculosis. This includes the exploration of novel diagnostic approaches, the creation of more effective and shorter treatment regimens, and the pursuit of new preventive measures, such as improved vaccines.
Conclusion
Tuberculosis remains a formidable challenge in the global health landscape, requiring a concerted and sustained effort to overcome. By addressing the multifaceted barriers to effective TB management, we can work towards a future where this preventable and treatable disease no longer poses a significant threat to the health and well-being of communities worldwide. Through collaborative actions, innovative approaches, and a steadfast commitment to equity and social justice, we can make meaningful progress in the fight against tuberculosis and improve the lives of millions.
For more information on water and sanitation services, community engagement, and advocacy efforts related to public health issues, I encourage you to visit the Joint Action for Water website.

