Unraveling the Molecular Landscape of Osteoarthritis Progression
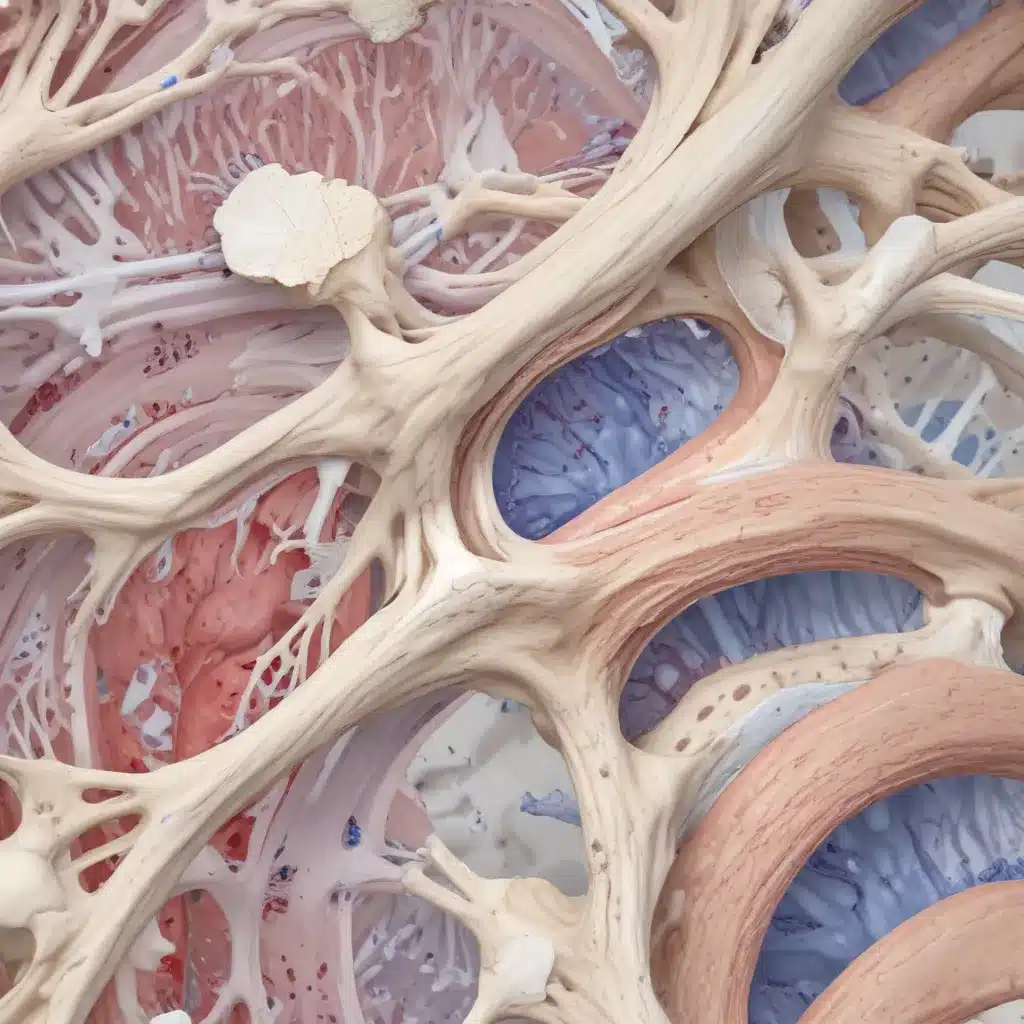
Osteoarthritis (OA) is the most common and debilitating joint disease worldwide, affecting millions of people. Despite extensive research, our understanding of the complex molecular mechanisms driving OA progression remains limited. However, a recent groundbreaking study has shed new light on this critical issue, leveraging the power of synovial fluid transcriptomics to uncover key insights.
The study, published in the prestigious journal Cell, delved deep into the transcriptional profiles of synovial fluid samples collected from OA patients across different disease stages. By employing advanced microarray analysis and bioinformatics approaches, the researchers were able to identify distinct gene expression patterns corresponding to the various grades of OA. This innovative approach provided a comprehensive view of the molecular changes underlying the progression of this debilitating condition.
Upregulation of Mineralization Genes Highlights Pathological Pathways
One of the most striking findings from the study was the consistent upregulation of two key genes – AMTN (Amelotin) and DKK2 (Dickkopf WNT Signaling Pathway Inhibitor 2) – as the disease advanced from early to late stages. AMTN, typically associated with enamel formation, was found to be significantly upregulated in the synovial fluid of patients with advanced OA, suggesting its potential role in the pathological mineralization processes occurring within the joint.
Similarly, DKK2, a known inhibitor of the Wnt signaling pathway crucial for bone remodeling, showed a marked increase in expression in late-stage OA. These findings point to the critical importance of dysregulated mineralization and disrupted bone homeostasis in the progression of osteoarthritis, opening up novel avenues for therapeutic intervention.
Inflammation and Cellular Dysfunction Emerge as Hallmarks of OA Advancement
The study’s comprehensive pathway analysis revealed another striking pattern – the upregulation of immune response, inflammation-related pathways, and cellular processes such as autophagy and programmed cell death as OA progressed from early to late stages. This suggests that the interplay between heightened inflammation and impaired cellular mechanisms, including mitochondrial dysfunction and disrupted autophagy, are key drivers of the disease’s severity.
Interestingly, the researchers observed that these inflammatory and cellular pathways were initially downregulated in the transition from early to moderate OA, potentially as a protective mechanism to prevent excessive inflammation. However, in advanced OA, these pathways were significantly upregulated, indicating a shift towards a high-grade, uncontrolled inflammatory state.
Unlocking the Potential of Synovial Fluid Biomarkers
By validating the expression of key genes identified in the transcriptomic analysis, the study further strengthened the significance of these molecular findings. The upregulation of AMTN, DKK2, and inflammation-related genes like IFIT2, IFIT3, and STAT1 in late-stage OA samples underscores their potential as valuable biomarkers and therapeutic targets.
Importantly, the researchers also quantified the AMTN protein levels in synovial fluid, revealing a substantial increase in advanced OA compared to early-stage disease. This highlights the translational potential of these discoveries, as protein-based biomarkers could provide a more direct clinical application for disease monitoring and targeted interventions.
Implications for Future Osteoarthritis Research and Treatment
The comprehensive insights gleaned from this synovial fluid transcriptome study have far-reaching implications for the future of osteoarthritis research and treatment. By unraveling the molecular landscape of disease progression, the findings shed light on the critical role of pathological mineralization, dysregulated inflammation, and impaired cellular processes in driving the severity of OA.
These discoveries pave the way for the development of novel, targeted therapies that can address the underlying mechanisms of the disease. Strategies aimed at modulating mineralization pathways, reducing inflammation, and restoring cellular homeostasis may hold promise for slowing or even halting the progression of osteoarthritis.
Furthermore, the identification of promising biomarkers, such as AMTN and DKK2, could revolutionize the way we approach OA diagnosis, monitoring, and personalized treatment. These molecular signatures could serve as valuable tools for early detection, disease stratification, and tailored therapeutic interventions, ultimately improving patient outcomes and quality of life.
By leveraging the power of synovial fluid transcriptomics, this groundbreaking study has opened up new frontiers in our understanding of osteoarthritis. As we continue to unravel the complex molecular mechanisms driving this debilitating condition, we are one step closer to ushering in a new era of more effective, personalized, and ultimately transformative approaches to managing this widespread and debilitating joint disease.
Harnessing the Potential of Synovial Fluid Biomarkers for Osteoarthritis Management
The remarkable insights gained from the synovial fluid transcriptome analysis highlight the immense potential of this biological fluid as a valuable source of biomarkers for osteoarthritis. Synovial fluid, being in direct contact with the affected joint tissues, provides a unique window into the molecular changes associated with the disease’s progression.
By focusing on the synovial fluid transcriptome, the researchers were able to identify key genes and pathways that are central to the pathogenesis of osteoarthritis. This approach holds significant advantages over relying on serum or plasma biomarkers, as synovial fluid more accurately reflects the local changes occurring within the joint environment.
The consistent upregulation of AMTN and DKK2, as well as the dysregulation of inflammatory and cellular pathways, underscore the critical importance of these molecular signatures in driving the severity of OA. Targeting these pathways and validating the identified biomarkers could pave the way for the development of novel, disease-modifying therapies that can effectively slow or even halt the progression of this debilitating condition.
Furthermore, the potential of synovial fluid biomarkers extends beyond therapeutic interventions. These molecular markers could also prove invaluable for early diagnosis, disease monitoring, and patient stratification. By identifying individuals at risk of developing advanced OA, clinicians can implement timely preventive measures and personalized treatment strategies, ultimately improving patient outcomes and quality of life.
Conclusion: Unlocking the Secrets of Synovial Fluid for Osteoarthritis Breakthroughs
The groundbreaking findings from the synovial fluid transcriptome study have truly transformed our understanding of osteoarthritis progression. By delving into the molecular landscape of this joint disorder, the researchers have uncovered a wealth of insights that hold the promise of revolutionizing the way we approach OA diagnosis, management, and treatment.
The discovery of key genes like AMTN and DKK2, as well as the identification of critical pathways involved in inflammation and cellular dysfunction, opens up new avenues for targeted therapeutic interventions. Harnessing the power of these synovial fluid biomarkers could lead to the development of novel, disease-modifying therapies that can significantly improve the lives of millions of individuals suffering from osteoarthritis.
As we continue to explore the vast potential of synovial fluid transcriptomics, we are poised to unlock even more secrets about the underlying mechanisms of this debilitating joint disease. By fostering collaboration between researchers, clinicians, and the broader healthcare community, we can translate these groundbreaking discoveries into tangible improvements in patient care and outcomes.
The future of osteoarthritis management is indeed bright, thanks to the transformative insights gleaned from this synovial fluid transcriptome study. By embracing these advancements, we can strive towards a world where OA is no longer a debilitating and incurable condition, but rather a manageable challenge that can be effectively addressed through personalized, targeted, and highly effective interventions.

